The FDA made a landmark decision on June 7, approving aducanumab (Aduhelm™, Biogen) for the treatment of Alzheimer’s disease. Aducanumab is the first new Alzheimer’s treatment in 17 years and the first ever shown to modify the course of the disease. Mark Roithmayr, Chief Executive Officer, and Howard Fillit, M.D., Founding Executive Director and Chief Science Officer, discussed on a June 9th ADDF webinar what this means for patients and for new drug development. They also touched on how ADDF’s 20-plus years of work in the field contributed to this approval, as well as to the most robust and diverse Alzheimer’s research pipeline in history.
Dr. Fillit began by discussing some of the controversy surrounding aducanumab and how the FDA approached the drug approval. “Because there was ambiguity in the study data, the FDA used a special approval pathway. Using Accelerated Approval, the FDA was able to make the drug available to today’s patients while ensuring we get more data from another gold-standard randomized, controlled clinical trial, which Biogen must complete as a condition of approval.”
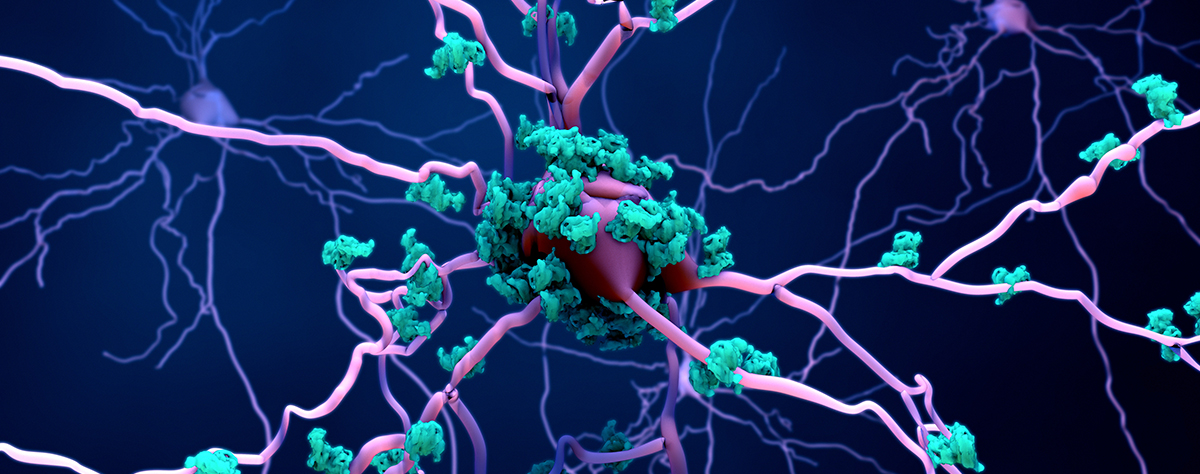
The ambiguity in the data — with only one of the two studies conducted showing that aducanumab slowed cognitive decline — set the stage for the FDA to rely on an Alzheimer’s biomarker for the first time. The Amyvid™ PET scan, which was developed and validated with support from the ADDF, was used to enroll patients with amyloid plaques in the aducanumab studies and to monitor the effectiveness of the drug.
The Accelerated Approval pathway requires that a drug “has an effect on a surrogate endpoint that is reasonably likely to predict clinical benefit.” In other words, the FDA believes that Amyvid test results showing clearance of amyloid plaques from the brain are likely to predict better patient outcomes — in this case, slowing cognitive decline.
The ADDF recognized early on that the path to FDA approval of Alzheimer’s treatments starts with biomarkers, an understanding that led to the creation of the Diagnostics Accelerator (DxA) in 2018. But even before the DxA kicked off, the ADDF supported other pioneering biomarker research, including the development of C2N Diagnostics’ PrecivityAD™ — which, in 2020, became the first ever commercially available biomarker blood test for Alzheimer’s disease. Measuring amyloid levels in blood samples, the test is widely available to help physicians with the early detection and diagnosis of Alzheimer’s. This test can correctly identify brain amyloid plaque status in 86% of patients and may, at some point, be an alternative to the more expensive Amyvid PET scan to help physicians and patients make informed treatment decisions.
A new era for Alzheimer’s clinical trials, with a pipeline primed to deliver results
Amyvid was developed with the kind of sophisticated trials Biogen ran for aducanumab in mind. The drug’s approval validates the ADDF drug development approach, prioritizing the application of known and new biomarkers in clinical trials to ensure that the right patients are enrolled and that the drug’s effect can be tracked.
While aducanumab and Amyvid focus on misfolded amyloid proteins, which are a hallmark of Alzheimer’s, these proteins are just one of many factors contributing to Alzheimer’s development and progression. More than 10 years ago, as big pharma took up the research mantle for effective drugs to work on amyloid plaques and tau tangles, ADDF decided it was time to shine a light on the biology of aging.
|
One specific area discussed was biomarkers for frontotemporal degeneration, or FTD. Biomarkers are especially important for FTD trials, which are notoriously difficult to complete because FTD is uncommon and patients are hard to diagnose accurately. FTD biomarkers, in Dr. Fillit’s words will “really up our game in clinical trials and accelerate drug development.” |
The biology of aging and its contribution to Alzheimer’s, which have been long championed by the ADDF, are now a mainstream research focus that is reflected in the drug development pipeline. More than half of the 120 drugs currently in Alzheimer’s drug development target biological processes other than misfolded proteins that go awry with aging — processes including inflammation, vascular problems, genetic alterations and metabolic dysfunction that contribute to Alzheimer’s.
“The ADDF has one of the most robust and diverse clinical trial investment portfolios in the world,” said CEO Mark Roithmayr. The ADDF is currently invested in 30 active trials, most of which are phase 2, and is actively engaged in finding more promising investments. The large number of trials in phase 2 and 3 development, plus the breadth of targets they cover, are the basis of Dr. Fillit’s optimism.
Who is the target patient population for aducanumab?
The FDA decision-making about aducanumab was front and center again as Dr. Fillit discussed who should consider treatment with aducanumab. The FDA provided no guidance about which patients are best suited for aducanumab treatment, approving it for use in anyone with Alzheimer’s disease. However, the clinical trials looked specifically at symptomatic patients in early stages of the disease. Dr. Fillit expects to focus on these patients in his own practice.
But, he said, this is very much a situation that requires shared decision making. Patients need to understand that treatment will not improve their condition, but at best will slow its progression. Treatment is by infusion once every four weeks, so patients and likely their caregivers will need to make a commitment to getting to an infusion center—travel time that will vary greatly based on a patient’s location—13 times a year.
And finally, the cost of treatment may prove a challenge for some, with no clarity yet about how Medicare, Medicaid and private insurance companies will approach paying for it. George Vradenburg, Chairman and Co-Founder of UsAgainstAlzheimer’s, is advocating on behalf of Alzheimer’s patients to get coverage not only for the treatment, but also for the PET scans that are so essential to identifying the right patients for it. Without insurance coverage for both, access to treatment will be inequitable based on patients’ financial resources.
Hope is here
Dr. Fillit closed by saying, “Alzheimer’s is not a one pathway disease, and we ultimately need drugs that target many biological processes so we can combine drugs into personalized treatments for each patient. The current pipeline is well positioned to give us this.”
Roithmayr added that this was as true before Monday’s FDA decision as it is today. “But one thing that this approval is sure to do is to attract more capital to this market — capital that the ADDF knows how to pinpoint at the most promising research areas.”
As exciting as it is to get the first approval in 17 years, ongoing financial investment will only speed what is to come, and what’s to come is even more exciting, said Dr. Fillit.