I recently saw an 80-year-old patient who was afraid he had Alzheimer's disease. He was a successful and active businessman, but had begun experiencing mild memory problems. Before he stepped into my office, he was already considering life-altering questions. “Will I have to quit the work that I love. How soon will I be disabled? How will my family take care of me?"
Diagnosing Alzheimer's
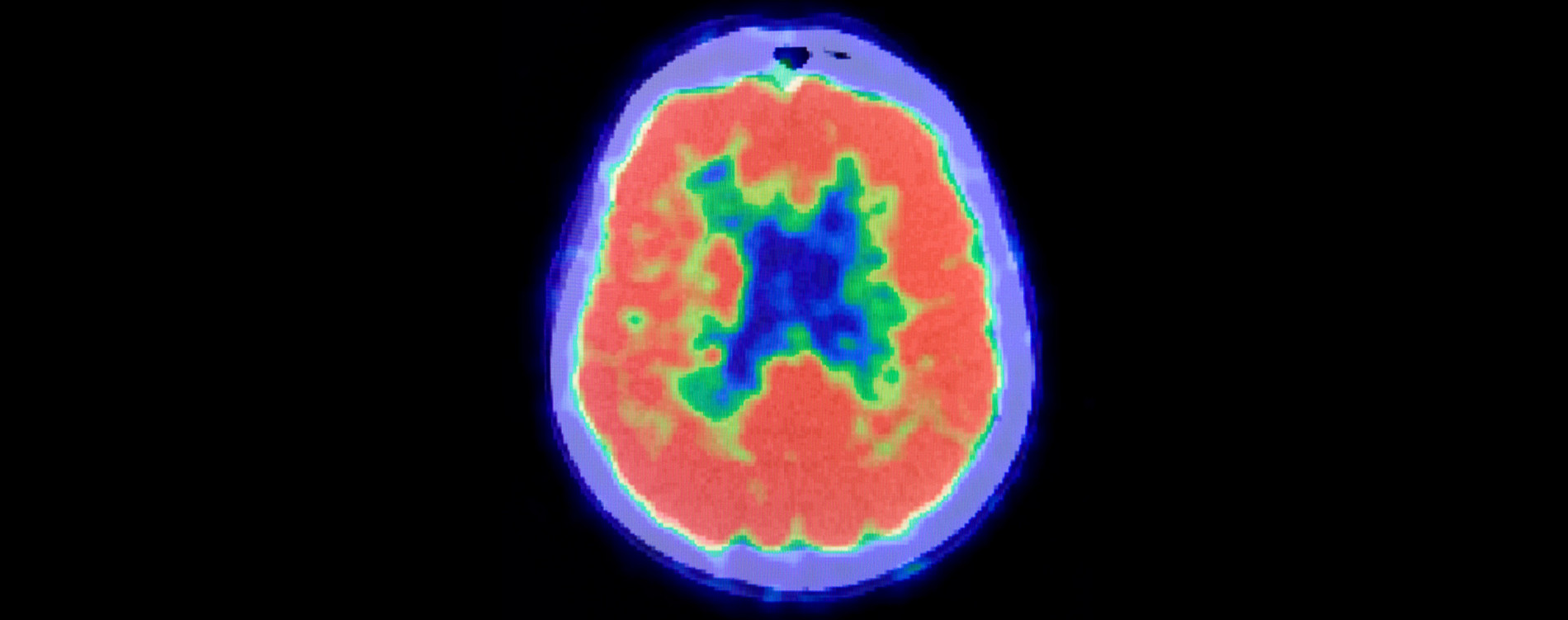
Up until 2012, the only way to conclusively diagnose someone with Alzheimer's was to wait until they died and conduct an autopsy—not very useful for patients who want answers. However, in 2012, the US Food and Drug Administration (FDA) approved a PET scan called Amyvid™ that detects beta-amyloid in the brain. It enables doctors to accurately diagnose Alzheimer's in living patients for the first time. Thanks to this test, we have found that up to 30% of patients diagnosed with Alzheimer's disease don't actually have it.
My patient underwent the Amyvid™ scan, which was negative. Instead, he had a condition called “mild cognitive impairment,” or MCI. About 50% of people with MCI go on to develop Alzheimer’s disease and will progressively get worse. But 50% of people with MCI won't get worse, and some may actually get better with proper assessment and care. The patient continued his work and his condition did improve with some lifestyle changes and medication.
In those cases where the test is positive, it helps physicians counsel people while they’re still able to prepare for the challenges that lie ahead. It is also critical for identifying appropriate and FDA-approved treatments for patients' symptoms once they progress to dementia.
Is Healthcare a Luxury?
The Amyvid scan is not currently approved for payment by Medicare or major insurance companies. My patient was able to afford it, but for most people, Amyvid™ is simply too expensive.
The FDA approved Amyvid™ as “safe and effective” in identifying beta-amyloid in the brain, but Medicare still has to approve payment for it and other diagnostic tests. In considering payment, Medicare seeks to determine the “value” of the test to individuals and society. The FDA asks whether a diagnostic tool is safe and does what it is reported to do. Medicare considers whether it can change health care outcomes. And while Medicare cannot decide to approve or disapprove payment for a test solely on the basis of the cost, in considering the value of a test, they can consider whether it is cost-effective from a societal perspective.
After weighing those considerations, Medicare did not approve payment for Amyvid™. This means most people won’t have access to it. Most experts, including those testifying to Medicare, argued that when used appropriately, Amyvid™ clearly has benefit for patients in accurate diagnosis, prognosis, and clinical care and that a negative test can have considerable value as well.
Medicare has proposed to only approve payment in research studies through a mechanism called “coverage with evidence development” or CED. This means that Amyvid™ will need to be tested in large, lengthy, and expensive research studies to prove its “clinical value.” No doubt this will take many years and millions of dollars, and if the value of the test is not clear, payment may again be denied. In the meantime, the vast majority of people will not be able to get the test.
Stifling Innovation, and Potential Cures
The case of Amyvid has repercussions for the drug discovery and development process. Developing a new drug or diagnostic tool takes over a decade and up to $2 billion. There is little incentive for researchers and pharmaceutical company to invest all that time and money on a new drug or test, succeed in getting FDA approval, and then have it go largely unused because of a Medicare denial. This possibility will clearly hinder innovation.
Conflicts in the bar for approval between the FDA, Medicare, and the insurance industry will likely become more acute under healthcare reform and increase in the coming years. As the largest payer in the United States, Medicare sets the course for the insurance industry, so its decisions affect everyone.
We have to find a way to make the criteria for approving Medicare payment more collaborative, while balancing the needs of patients and society. Current quality of care and future research on the development of new diagnostic tests and drugs depend on it.
Howard Fillit, MD is the Founding Executive Director and Chief Science Officer at the ADDF.